To Know Your Treatment Options
What is Kidney Transplantation?
Step 1: Making an Informed Decision
Step 3: Finding a Live Kidney Donor
Transplant Eligibility & the Kidney Matching System
To Know Your Treatment Options / Step 3: Finding a Kidney Donor / Transplant Eligibility & the Kidney Matching System
People of all ages with advanced kidney failure can get a transplant. Individuals may be considered for pre-emptive kidney transplantation if their measured or calculated glomerular filtration rate (GFR) is less than 15 mL/minute on two occasions and there is evidence of progressive and irreversible decline in kidney function over the past 6–12 months.
Patients must complete a thorough medical and psychosocial evaluation to be considered for a kidney transplant. Whether someone is a good candidate for transplant depends on a number of factors, such as general health, history of heart disease, cancer, obesity, emotional or psychological factors, and evidence of adherence to a treatment plan.
In many cases, people who are older or have health conditions like diabetes and high blood pressure can still have successful kidney transplants. Recipients may be asked to do some things that can lessen certain risks and improve the outcomes of their transplant. For example, they may be asked to lose weight or quit smoking.
Only medical and logistical factors are taken into consideration for matching organs with recipients. Personal or social characteristics such as status, income or race do not play a role in transplant priority. However, due to social and cultural factors (eg. willingness to ask for a volunteer donor, access to healthcare services), those in ACB communities may spend longer on waiting lists. This is why it is important to raise awareness about kidney transplants in ACB communities!
Before a donor organ is selected, transplant candidates on the waiting list are screened for factors like matching blood type, height, and weight. Proper organ size is critical to a successful transplant.
The Kidney Matching Process
There are three main blood tests to determine if a recipient and a potential donor are a kidney match: blood typing, tissue typing and cross-matching.
Blood Typing
- Determines if the transplant recipient’s blood is compatible with the potential donor’s blood. The following blood types are compatible:
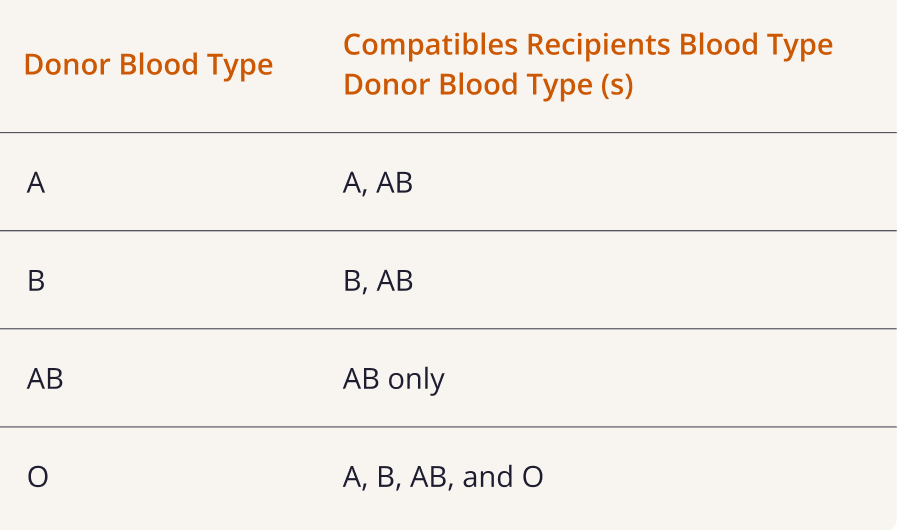
If blood types are not compatible, the donor still may be able to donate directly to the recipient using treatments that lower the recipient’s blood antibody levels. In addition, the donor may consider donating through a paired exchange program.
For more information see Step 1: Process of Getting a Transplant
Tissue Typing
If the donor and recipient blood types are compatible, the donor will take the next test, tissue typing, which consists of two blood tests.
- Tissue (HLA) type blood test
- Determines the tissue (HLA) type of the recipient and the potential donor to see how well they both match. A parent and child have at least a 50% chance of matching, siblings could have a 0-100% match, and unrelated donors are less likely to match
2. Measures antibodies to HLA blood test
- This test is done for the recipient only and is repeated frequently before, during, and after transplant.
- The immune system can make antibodies against a blood/tissue type after a blood transfusion, minor surgery, infections, or pregnancy. A kidney won’t be a match if the recipient has antibodies against the donor’s tissue type.
- The calculated panel reactive antibody (cPRA) tells you what percentage of potential living donors you are incompatible with based on your antibodies. People with a cPRA higher than 95% are called highly sensitized, and have a much harder time finding a match. However, they can register in the Canadian Blood Services’ Highly Sensitized Patient Program to be matched with a deceased donor.

Cross-Matching
Serum crossmatch blood test
- This is a blood test that is done multiple times, including right before the transplant surgery.
- To do the test, white blood cells from the donor are mixed with the patient’s serum, a part of the blood. If the serum has antibodies against the donor’s cells, the transplant cannot take place due to high rejection risk.
Toronto General Living Donor Program
If a recipient and donor are partially matched, transplant can still occur through:
- Living Donor Paired Exchange Program. Two donors switch their recipients so that the respective recipients can still receive a kidney.
- List Paired Exchange Program. A donor will donate a kidney anonymously to the kidney transplant waiting list to Toronto General Hospital. This is done in exchange for their intended recipient receiving the next deceased donor kidney from a waitlist.
Kidney Transplant Resources
Now that you know more about the kidney matching process. It is time to move on to Step 4: Receiving a Kidney Transplant & Managing Your Care
